Last updated: April 25, 2023
Article
Leptospirosis
(This page is part of a series. For information on other illnesses that can affect NPS employees, volunteers, commercial use providers, and visitors, please see the NPS A–Z Health Topics index.)
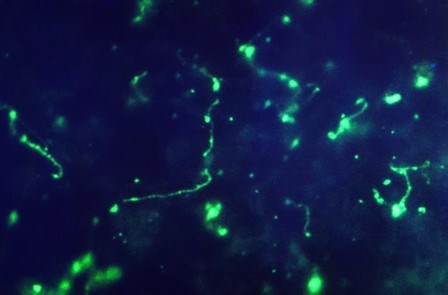
Humans: Leptospirosis is a zoonotic disease caused by spiral-shaped bacteria within the genus Leptospira. The bacteria are excreted in the urine of infected animals. In suitable environments (e.g., freshwater lakes, rivers, muddy or moist soils), the bacteria can survive for weeks to months. Humans can become infected with the bacteria in several ways. The bacteria can enter the body through a break in the skin; via penetrating the mucous membranes of the eyes, nose, or mouth; or through the gastrointestinal tract following ingestion. Therefore, human infection may occur following direct contact with urine from an infected animal, contact with water or soil contaminated with the bacteria, and ingestion of contaminated food/water. During 2014 – 2018, U.S. states and territories reported about 100-200 human cases annually, with a high proportion of cases reported from Puerto Rico and Hawaii.In humans, leptospirosis can be asymptomatic or may resemble the flu or other illnesses, with symptoms that can include but are not limited to fever, headache, chills, muscle aches, reddened eyes, gastrointestinal illness (e.g., vomiting, abdominal pain, and diarrhea), and a rash. Symptoms vary widely, can involve the brain, lungs, kidney, liver, or eyes, and can become severe and result in death. Leptospirosis may also occur in two phases. People typically become sick between two days and four weeks after exposure to the bacteria, and illness may last from a few days to several weeks. Leptospirosis is treatable with appropriate antibiotics given promptly after symptoms are noted. Vaccination is not available for humans currently.
Animals: Leptospirosis infections can occur in almost any mammalian species. Infected animals may show no signs of illness or may become seriously ill or die. Dogs, cattle, horses, sheep, goats, and swine are the domestic species most frequently infected. Rodents (e.g., beavers, squirrels, rats, and mice), raccoons, skunks, deer, feral pigs, and marine mammals are among the many wildlife species that can become infected. Animals harbor the Leptospira bacteria in their renal system and can shed the bacteria continuously or intermittently in urine for years. Vaccines for dogs and some livestock are available as recommended by an animal health professional.
Environment: Leptospirosis occurs worldwide but is most common in tropical areas with higher heat and humidity. The Leptospira bacteria can contaminate water or muddy soils, where people may be exposed during outdoor recreational activities including swimming, wading, fly fishing, kayaking, and rafting in lakes and rivers. Climate change, population growth, and habitat invasion have increased human and animal exposure to Leptospira bacteria. Leptospirosis outbreaks have also been associated with natural disasters such as hurricanes and floods that result in standing water.
PREVENTION
- Avoid recreational activities in non-chlorinated water (e.g., swimming in lakes) if you have fresh cuts or abrasions through which Leptospira bacteria could enter.
- Avoid swallowing water and keep your head above water during outdoor aquatic recreational activities, when possible, to protect the mucous membranes of your mouth, nose, and eyes from contact with potentially contaminated water.
- Avoid bathing or wading in floodwater.
- Wear protective clothing and footwear, such as rubber boots, if you may be exposed to floodwater. These may be a good idea, in general, when recreating/working in water or soil in parks, particularly if there is a concern that the water or soil may be contaminated.
- Boil untreated water prior to drinking.
- As a general practice, avoid contact with rodents and their droppings.
- Within buildings, keep rodents and other pests under control by sealing rodent entry points and storing food in secure containers to minimize rodent attractants.
- Follow veterinarian recommendations to vaccinate pet dogs and livestock (i.e., cattle, swine, and horses) against leptospirosis.
- For employees: Wear appropriate personal protective equipment (gloves) when trapping and handling rodents as part of your job responsibilities.
- If you become ill following a potential exposure, contact your healthcare provider and let them know of your concern. Also, please report any confirmed illnesses to the NPS Office of Public Health (e-mail us) as directed in the “Disease Reporting” guidance below.
- Report concerns about sick or dead wildlife to the park resource manager and the Wildlife Health Branch at e-mail us.
- Report information about rodents inside buildings to park staff or a supervisor immediately. Exclude rodents from areas in which people live, work, and eat.

OTHER RESOURCES:
- CDC Diseases Spread by Rodents
- CDC Leptospirosis Website
- USGS Safe Work Practices for Working With Wildlife
NPS-SPECIFIC PUBLICATIONS:
- Adjemian J, Weber IB, McQuiston J, et al. Zoonotic infections among employees from Great Smoky Mountains and Rocky Mountain National Parks, 2008-2009. Vector Borne Zoonotic Dis. 2012;12(11):922-931. doi:10.1089/vbz.2011.0917
