Last updated: November 6, 2024
Article
Rabies
(This page is part of a series. For information on other illnesses that can affect NPS employees, volunteers, commercial use providers, and visitors, please see the NPS A–Z Health Topics index.)
CDC
Rabies is a preventable viral infection of mammals that is almost always fatal once symptoms develop. The virus has been identified in animals in all 49 continental states; only Hawaii is rabies-free.
Humans: Rabies is generally transmitted through the saliva of infected animals (e.g., bats, raccoons, skunks, coyotes, feral cats) through a bite or a scratch. The virus causes a range of symptoms, which often begin as behavioral changes or nonspecific symptoms (fever, headaches, nausea, vomiting) and then progress to neurologic symptoms and death. The incubation period between the initial exposure (bite or scratch) and the appearance of symptoms can last weeks to months. Rabies is preventable if medical treatment, called post-exposure prophylaxis (PEP), is given before symptoms of rabies develop. About 60,000 Americans receive PEP each year, which contributes to the low number of human rabies cases in the U.S. (only 1–3 cases are reported annually). Globally, however, rabies is thought to cause approximately 59,000 deaths annually. Rabies PEP for most people who have not previously been rabies-vaccinated consists of IV administration of rabies immunoglobulin (antibodies) and a series of four shots over the course of two weeks. CDC recommends that individuals who are at elevated risk of rabies exposure because of their travel plans or their professions (e.g., veterinarians, wildlife biologists) be pre-vaccinated against rabies (pre-exposure prophylaxis). If an exposure occurs in someone who has been pre-vaccinated, rabies PEP should still be given; however, it is usually a much simpler and less costly regimen than among those who were not previously vaccinated.
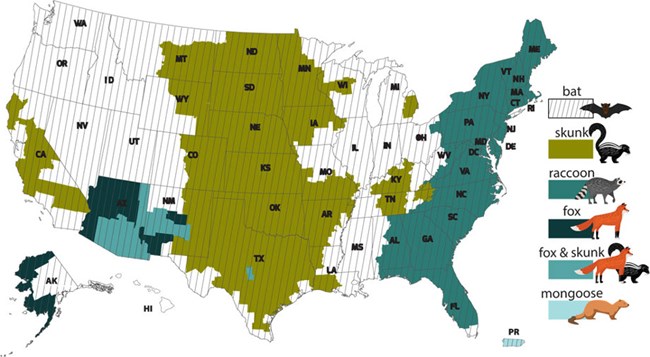
Animals: Rabies affects only mammals and is fatal for pets and wildlife as well as humans. Although terrestrial rabies was first introduced into the lower 48 United States through domestic dogs, today more than 90% of all animal rabies cases reported annually to the CDC occur in wildlife. Animals infected with rabies can lose their fear of humans and seem sleepy or confused or aggressive; rarely some animals may not have any obvious signs of being infected with rabies. Multiple variants of rabies virus have been identified in the United States, including raccoon, red fox, gray fox, skunk, coyote, and several bat variants. Although variants are usually associated with a specific reservoir species, they infect other species as well. Although less than 1% of bats in nature are infected with rabies, bat variants of rabies are found in most areas of the United States and are responsible for the majority of human deaths from rabies. Although dog rabies remains common in many countries, the canine strain of rabies has been eliminated from the United States and dogs make up only about 1% of rabid animals reported each year in the U.S.
Environment: The rabies virus is transmitted via the saliva of an infected animal or person. Rabies virus is fragile, does not live long in the environment, and is killed by desiccation (drying out), sunlight, and common disinfectants.
PREVENTION
- Enjoy wildlife from a distance. Do not touch or pet wild animals.
- Alert a park ranger if you see a sick or strangely acting animal. Do not approach it.
- Ensure housing and overnight dwellings (tents or cabins) are sealed off from the outdoors and that there are no small openings through which bats or other wildlife can enter. If this is not possible, sleeping under mosquito nets may prevent bats from contacting sleeping persons.
- Educate children about animals and rabies, as children are most at risk.
- Ensure your pets are up to date on vaccinations, especially for rabies, to protect them and your family.
- Talk to a medical provider about pre-exposure vaccination if you work with animals that could have rabies or are traveling to an area of the world where rabies is common.
- Consider the following to be a potential exposure:
- Direct or suspected contact with any wildlife or unfamiliar animals, especially any bites or scratches
- Waking up with a bat in the room (in this case, please reference the Bats in Buildings flowchart included in the Resources below)
- If a potential rabies exposure occurs,
- Immediately wash any animal bites or scratches with soap and water.
- Notify a park ranger of the incident. They can collect the animal so it can be tested.
- Contact your healthcare provider or local health department as soon as possible about whether post-exposure prophylaxis is needed.
- Please report any exposures or confirmed illnesses to the NPS Office of Public Health (e-mail us) as directed in the “Disease Reporting” guidance below.
- Report concerns about sick or dead wildlife to the park resource manager and the Wildlife Health Branch (e-mail us).

- Bats in Buildings Flowchart (updated January 2024)
- NPS Action Steps to Prevent Human Rabies Following Animal-Human Contact (Updated May 2024)
- NPS internal webpage on bats and people (restricted access)
- NPS external webpage on bats and people
- CDC Rabies webpage
- Rabies Advisory Committee on Immunization Practices (ACIP) Vaccine Recommendations
- Cote A, Wallace RM, Jackson DA, et al. Evaluating the public health response to a mass bat exposure-Wyoming, 2017. Zoonoses Public Health. 2019;66(5):504-511. doi:10.1111/zph.12585
- Pearce EA, Farney AN, Banks L, Harrell AJ. Multi-Patient Rabies Exposure on a Colorado River Rafting Expedition: Urgent vs. Emergent Transport Decision Making in an Austere Setting. Prehosp Emerg Care. 2018;22(2):276-279. doi:10.1080/10903127.2017.1367445
- Cote A, Guagliardo SAJ, Tran CH, et al. Notes from the Field: Assessing Rabies Risk After a Mass Bat Exposure at a Research Facility in a National Park - Wyoming, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(10):313-314. doi:10.15585/mmwr.mm6710a7
- Lu H, McComas KA, Buttke DE, Roh S, Wild MA. A One Health Message about Bats Increases Intentions to Follow Public Health Guidance on Bat Rabies. PLoS One. 2016;11(5):e0156205. doi:10.1371/journal.pone.0156205
