Last updated: July 20, 2023
Article
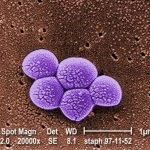
Staph Infections, including MRSA
(This page is part of a series. For information on other illnesses that can affect NPS employees, volunteers, commercial use providers, and visitors, please see the NPS A–Z Health Topics index.)
CDC
Staphylococcus aureus is a bacterium that is commonly found on human skin and can cause a variety of illnesses in humans ranging from skin infections to pneumonia to bloodstream infections (sometimes called “Staph” infections). Some of these Staph bacteria have become resistant to antibiotics previously used to treat them – these resistant bacteria are called “Methicillin-Resistant Staphylococcus Aureus” or “MRSA”. MRSA is one of many organisms that are developing resistance to antimicrobial medications. Although baseline levels of resistance in the environment can be expected, one of the main drivers of resistance is the overuse and misuse of antimicrobials in people, animals, and crops. Antimicrobial resistance is an emerging global threat and a true One Health issue.
Humans: Studies show that 1 in 3 people carry Staph on their skin or in their nose, and 2 in 100 people carry MRSA. People can carry, or are “colonized” with these bacteria without necessarily having illness. The bacteria are spread through direct skin-to-skin contact or by touching surfaces that are contaminated. The bacteria often cause infections at the site of non-intact skin. Anyone can get MRSA infections, but athletes, daycare and school students, military personnel in barracks, and patients in hospital or nursing home settings are at higher risk. Most MRSA skin infections appear as a bump that might be red, swollen, painful, warm to the touch, full of pus or other drainage, and sometimes accompanied by a fever. Sometimes, people mistake these infections for a spider bite.
Animals: Staph aureus and MRSA can colonize and infect animals as well, and has been identified in dogs, cats, horses, pigs, cows, and others. MRSA isolates have also been found among wildlife. The bacteria can spread back and forth between animals, or between animals and humans.
Environment: MRSA can survive on some surfaces for up to weeks. It spreads to people through contact and causes infections when it gets into a cut, scrape, or open wound. The EPA maintains a list of disinfectants thought effective against MRSA (see List H).
PREVENTION
- Wash hands frequently, especially after exercise. Use soap and water. If soap and water is not available, use an alcohol-based sanitizer that contains at least 60% alcohol.
- Keep cuts, scrapes, and wounds clean and covered until healed.
- Avoid sharing personal items such as towels and razors.
- If you suspect you might have a MRSA skin infection, cover it, and contact your healthcare provider. Staph infections, including MRSA, can be treated. Early treatment is important.
- Wash clothes, sheets, and towels according to the clothing and detergent manufacturers’ instructions.
- Throw any bandages and tape into the trash.
(Last updated 7/20/2023)

